24.4.2021
International Webinar Series Episode 1: Breast Cancer
The Centre for Cancer Research and the Centre for Stem Cell Research, FMHS UTAR, successfully organised the International Webinar Series Episode-1 “Breast Cancer” on 24 April 2021, 10 AM – 12.30 PM (Malaysia time: GMT +8) via the Zoom meeting platform. Four distinguished speakers were invited to share their knowledge on the latest advancement in research and clinical practice in breast cancer management. A total of 75 participants (undergraduate & postgraduate students, researchers, specialists, and allied health staff) from the various institutions and universities participated in a fruitful discussion and Q&A session of the event.
The first speaker was Professor Dr Leong Chee Onn, from the School of Pharmacy and Health Sciences, Department of Life Sciences, International Medical University, Malaysia and Deputy Director (Research), Institute for Research, Development and Innovation, International Medical University, Malaysia. Prof. Dr Leong shared the work done by his group on the targeting of breast cancer stem cells by using high-throughput chemical library screening.

Dr Noor Ezmas Mahno from the Department of Surgery, Kulliyah of Medicine, International Islamic University Malaysia then updated the participants regarding the current management of early breast cancer in Malaysia.
Following this, Dr Kyaw Toe, staff surgeon at the Breast Unit at North Tees and Hartlepool NHS Trust, shared the experience of his institution in terms of breast conserving surgery. Dr Kyaw talked about the principles of breast conserving surgery and how it was done in the past and the current practice.

Finally, Clinical Associate Professor Dr Myo Oo, from the Department of Population Medicine, Faculty of Medicine & Health Sciences, Universiti Tunku Abdul Rahman, talked about implementation research and its importance in breast cancer research.

A Q&A session followed the talk where each speaker took turns to answer some questions from the participants. The Q&A session was moderated by Associate Professor Dr Leong Pooi Pooi and Dr Fann Rui Jeat.

Professor Dr Alan Ong Han Kiat, Chairperson of the Centre for Stem Cell Research, gave the closing remarks on behalf of the webinar organising committee. He thanked the speakers and participants for the successful webinar. He acknowledged the challenging aspects of breast cancer management but also the many opportunities and need for good research that will pave the way towards better treatment and management for a brighter future for breast cancer patients. Prof. Dr Alan concluded the webinar by highlighting the on-going donation drive for setting up a not-for-profit private hospital by UTAR in Kampar and encouraged participants to donate to the hospital’s building fund.

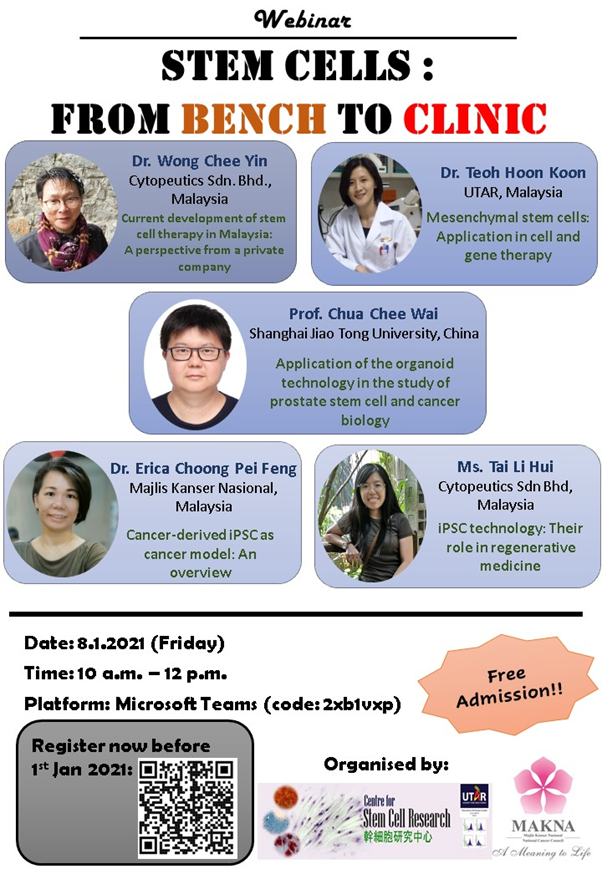
8.1.2021
Missed out the webinar entitled "Stem Cells: From Bench to Clinic"?
Just click to view the videos:
Cancer-Derived iPSC as Cancer Model: An Overview, by Dr. Erica Choong
iPSC Technology: Their Role in Regenerative Medicine, by Ms. Tai LiHui
Mesenchymal Stem Cells: Application in Cell and Gene Therapy, by Dr. Teoh Hoon Koon
Q & A session with the speakers and the Dean of UTAR Faculty of Medicine & Health Sciences:
Prof. Chua Chee Wai
(1) Prof. Chua, as you are engaged in lab works, do you still treat patients in the hospital as a urologist?
(2) How long does it take to generate an organoid and also the maintenance too?
(3) How thick is an organoid formed from under the surface of culture? In drug testing, how do you ensure drugs given are exposed to all organoids at different layers of thickness?
(4) Could you please share your experience on organoid culture for first-timer?
Prof. Cheong Soon Keng
Dr. Teoh Hoon Koon
(1) I would like to know your opinion on MSC differentiated from iPSCs. Can these MSCs-iPSCs replace the actual MSCs in clinical therapy?
(2) Since MSC has limitation as there are possibilities of pro-tumour activity, would you mind to share on how to ensure the MSC treatment will not trigger this?
(3) I am wondering, have you guys thought of using MSC to co-culture with cancer to assess whether 1. If the cancer would promote the differentiation of MSC into cancer associated fibroblast or 2. If they could suppress the growth of the cancer cells?
Dr. Erica Choong
(1) Have you tried to generate a specific type of cancer from iPSC?
(2) Do you think the loss of tumorigenicity of cancer upon reprogrammed into iPSC is something to do with the switching of tumor cells back into more "normal state"?
(3) Could these "iPSCs" remove the tumor cells in the tumor microenvironment?
(4) Since you are generating cancer-derived iPSC, what do you think of cancer-derived iPSC potential in research or in clinical study?
Dr. Wong Chee Yin
(1) For the use of MSC to treat various pathological conditions, once the patients show an improvement, would you guys continue injecting MSC to the patients to further improve the condition? When you stop treating the patients, would the pathological condition appear again?
(2) Can you share how you scale up the MSC numbers for clinical usage? As we know, MSC can be hampered by their limited proliferative rate.
Ms. Tai LiHui
(1) What would be the major advantage of using iPSC compared to MSC?
(2) In
your opinion, how much can the MSC-iPSC can differ from the actual MSC? In
terms of morphology and the expressions?